Introduction
- Amid the pandemic, another challenge has been thrown up before mankind as antibiotic resistance has emerged as one of the biggest threats to global health, food security, and development today.
- In fact, many recent studies have said that the world stands at the edge of a 'post-antibiotic era'.
- Under this, resistance can spread everywhere and create untreatable infections with antibiotic resistance which can affect anyone, of any age.
- Over the past years, the use and misuse of antimicrobials has increased the number and types of resistant organisms.
- Consequently many infectious diseases may one day become uncontrollable.
- With the growth of global trade and travel, resistant microorganisms can spread promptly to any part of the world.
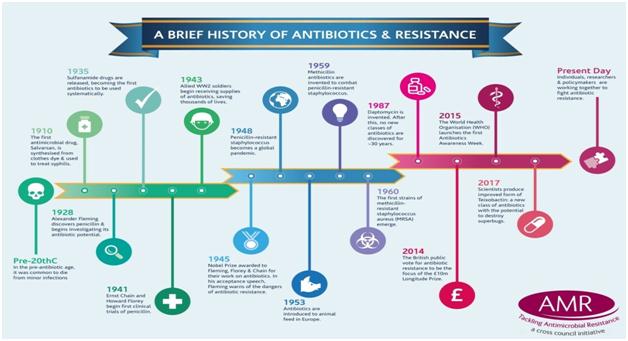
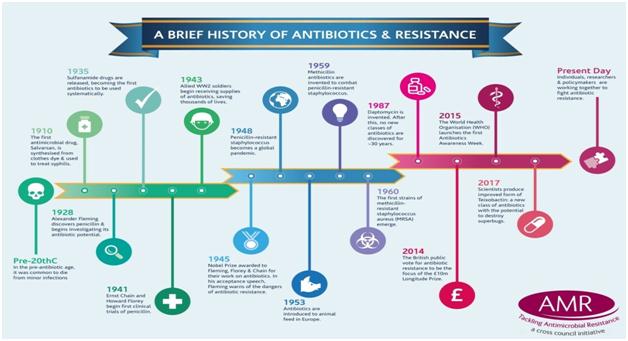
Antimicrobial resistance
- Antimicrobial Resistance (AMR) occurs when bacteria, viruses, fungi and parasites change over time and no longer respond to medicines making infections harder to treat and increasing the risk of disease spread, severe illness and death.
- As a result of drug resistance, antibiotics and other antimicrobial medicines become ineffective and infections become increasingly difficult or impossible to treat.
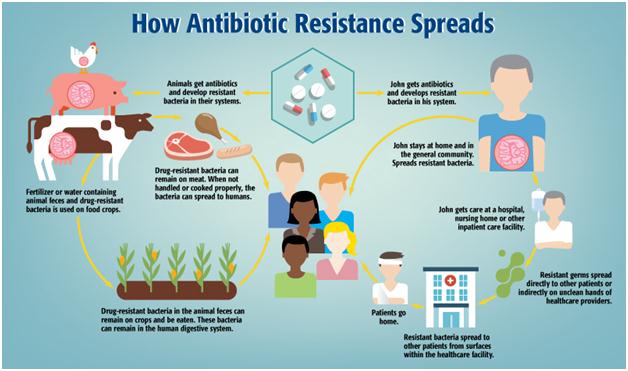
- AMR occurs naturally over time, usually through genetic changes. Antimicrobial resistant organisms are found in people, animals, food, plants and the environment (in water, soil and air).
- Transmission: They can spread from person to person or between people and animals, including from food of animal origin.
- Main drivers: The main drivers of antimicrobial resistance include
- the misuse and overuse of antimicrobials
- lack of access to clean water, sanitation and hygiene (WASH) for both humans and animals
- poor infection and disease prevention and control in health-care facilities and farms
- poor access to quality, affordable medicines, vaccines and diagnostics; lack of awareness and knowledge
- lack of enforcement of legislation
Important facts
- Antimicrobial resistance (AMR) is a global health and development threat. It requires urgent multisectoral action in order to achieve the Sustainable Development Goals (SDGs).
- WHO has declared that AMR is one of the top 10 global public health threats facing humanity.
- Misuse and overuse of antimicrobials are the main drivers in the development of drug-resistant pathogens.
- Lack of clean water and sanitation and inadequate infection prevention and control promotes the spread of microbes, some of which can be resistant to antimicrobial treatment.
- The cost of AMR to the economy is significant. In addition to death and disability, prolonged illness results in longer hospital stays, the need for more expensive medicines and financial challenges for those impacted.
- Without effective antimicrobials, the success of modern medicine in treating infections, including during major surgery and cancer chemotherapy, would be at increased risk.
|
What causes drug resistance?
- Drug resistance is a natural evolutionary phenomenon.
- When microorganisms are exposed to an antimicrobial, the more susceptible organisms succumb, leaving behind those resistant to the antimicrobial.
- They can then pass on their resistance to their offspring.
- Antimicrobials – including antibiotics, antivirals, antifungals and antiparasitics – are medicines used to prevent and treat infections in humans, animals and plants.
- Antibiotics: These are medicines that help stop infections caused by bacteria. They do this by killing the bacteria or by keeping them from copying themselves or reproducing. The word antibiotic means “against life.
|
Why antibiotics are an important pillar of modern medical practice?
- Antimicrobial agents have played a critical role in reducing the burden of communicable diseases across the world.
- The advent of antibiotics significantly increased the chances of surviving serious bacterial infectious diseases.
- Moreover, antibiotic therapy enabled the development of chemotherapy, organ transplantation, surgery in general and a wide range of medical interventions over the past eight decades.
- Effective antibiotics are the cornerstone of modern medical practice.
- With an increased focus on AMR globally and in India, the Indian Council of Medical Research and other stakeholders made important steps to introduce antimicrobial stewardship to rationalise antibiotic prescriptions in hospital settings.
Antimicrobial resistance in India
- Poor availability and utilisation of diagnostics : In India, poor availability and utilisation of diagnostics, insufficient antibiotic stewardship and compromised infection control both in community and hospital settings result in over-reliance on and over-use of antimicrobials.
- Weaknesses in health systems :With weaknesses in health systems and public health capacities in many countries, addressing the challenge of excessive use while at the same time assuring sustainable supply of essential antibiotics is key to make health systems resilient to both COVID-19 and antimicrobial resistance.
- Balancing excessive and inappropriate use: The government needs to balance excessive and inappropriate use, a key driver of antibiotic resistance, while ensuring live-saving medicines are available to those who need them.
With AMR, will India achieve its health targets?
- AMR can also cause a significant setback to India achieving its stated health targets.
- India has set a target that by 2025, it will eliminate all case of tuberculosis. India had an estimated 130,000 drug-resistant TB cases in 2018.
- However, only 44 per cent or around 58,347 of the estimated multidrug-resistant cases were diagnosed.
- AMR is certainly going to impend the progress made through dedicated research, investment and hard work of our scientists, medical professionals, and healthcare workers and needs immediate attention of the regulators.
- There are several economic costs that come with AMR as well.
- From costlier treatment and medicines, lengthier stays in the hospital, complicated procedures, and requirement of more intensive care – all these steadily add to the catastrophe.
- Naturally, the impact would be felt more intensely by low and middle-income countries, furthering deepening economic inequality as well as the resource gaps.
|
Flaws in medical fraternity
- Consumption of antibiotics is the key driver of resistance. Effective management of this limited resource will ensure antibiotics are only used when appropriate and necessary.
- Lack of formal training: Many medical practitioners lack formal training in India and 70 per cent of primary healthcare is delivered by such individuals. Sales companies target both doctors as well as those acting in a medical capacity without required qualifications.
- Incentivizing the sale of antibiotics: They may be given gifts, such as medical equipment, televisions, travel or cash not to switch to competitors or to incentivise the sale of antibiotics to dispensers.
- Biased and commercially motivated information: Pharmaceutical sales representatives are a key source of updates and information for prescribers, but the information they provide may be biased and motivated by commercial considerations to promote antibiotic sales.
- Unqualified health workers: Efforts in India to address the high levels of unqualified health workers by offering training courses will need to be monitored closely for success.
- Even trained doctors worry that patients may not return if they are not prescribed antibiotics. Trainee doctors need more training on antimicrobial resistance (AMR). Standard treatment guidelines are either lacking or may have been developed by different authorities for the same conditions.
- These guidelines only partially fulfil the World Health Organization (WHO) recommendations. Consensus on treatment recommendations, tailored to local environments, is the need of the hour.
- The sale of antibiotics without a prescription is prohibited under Schedule H1, which has been supported by the red line campaign. But it is not widely enforced.
- Easy accessibility: Antibiotics continue to be easily accessible and self-medication rates are 73 per cent in some parts of India. The lack of access, due to geographical distance or affordability, to medical professionals and prescribers, in rural areas of India, leads 50 per cent of people to buy antibiotics directly from the pharmacy as a first choice.
How coronavirus disease threatens to undermine the efforts of antibiotic thereapies?
- The novel coronavirus disease (COVID-19) threatens to undermine these efforts by creating conditions that lead to inappropriate use of antibiotics.
- Broad-spectrum antibiotic use and overuse is common among COVID-19 patients and prescribing is often based on clinical presentation rather than laboratory markers; besides that, differentiation between bacterial and viral pneumonia can be difficult even with availability of laboratory tests, particularly for severe cases.
- The World Health Organization is concerned AMR will be further fuelled by the inappropriate use of antibiotics during the COVID-19 pandemic.
- Only a small proportion of COVID-19 patients may need antibiotics to treat subsequent or concomitant bacterial infections and the organisation has issued guidance specifically to not provide antibiotic therapy or prophylaxis to patients with mild COVID-19 or to patients with suspected or confirmed moderate COVID-19 illness unless there is a clinical indication to do so.
Measures to control antimicrobial resistance
Clean up first
- Swachh Bharat Mission: Beyond access to effective antibiotics, reductions in India’s mortality from infectious diseases will be brought about by improvements in vaccination coverage, access to clean water, adequate sanitation and improved hygiene. Half of the south Asian population lacked access to basic sanitation in 2018. The Swachh Bharat Mission in India has improved access to toilets in many areas.
- However, efforts must be made to bring about behavioural changes so that people use these toilets.
- One estimate found that improvements to the infrastructure required for and access to clean water, adequate sanitation and quality hygiene in India could result in a reduction of 590 million diarrheal cases by 2020 that would have been treated with antibiotics.
- Vaccination has been shown to reduce the transmission of AMR infections and the volume of antibiotics consumed due to both, appropriate treatment of bacterial infections and inappropriate treatment of viral infections.
- Mission Indradhanush: India has undertaken many activities like Mission Indradhanush — to address low vaccination coverage — strengthened micro-planning and additional mechanisms to improve monitoring and accountability.
Integrating stewardship into pandemic response
- Need of guidelines: It is important for countries like India to introduce guidelines to define indications and conditions of antibiotic use in COVID-19 patients and encourage treatment providers follow the principles of antimicrobial stewardship.
- The development, updating and dissemination of evidence-based guidelines at the country level is urgently needed to support antimicrobial stewardship interventions specific to COVID-19.
- Availability of diagnostic tests :In addition, it is crucial to make available diagnostic tests to help in the identification of bacteria and their resistance patterns such as culture / Aspartate aminotransferase or equivalents and the diagnostic capacity to differentiate between simple COVID-19 infections from those including co-infections or alternative diagnosis (like imaging, procalcitonin, etc).
- Systematic testing of severe COVID-19 patients: Concrete measures such as systematic testing of severe COVID-19 patients with suspected bacterial co-infections are needed to better integrate antimicrobial stewardship into the pandemic response.
- The increased focus on COVID-19 and the restrictions imposed by the pandemic have affected aspects of the health system response to AMR such as surveillance and training. These aspects have to be preserved and strengthened.
- Through proper microbiology diagnostic capacity, it is possible not only to provide better targeted individual patient care but also conduct proper surveillance of antibiotic resistance: Health systems will be able to monitor the threat of antimicrobial resistance that lurks behind the pandemic.
Achieving sustainable access antibiotics
- The Indian drug regulatory authority’s reaction to impose export restrictions on active pharmaceutical ingredients (including antibiotics) during the COVID-19 pandemic to deal with possible shortages at the domestic level could have further threatened continuity of supply.
- Managing and mitigating the risks associated with the competition for scarce resources, like essential antibiotics, during a pandemic and beyond requires international cooperation and global solidarity.
- Without international mechanisms to achieve sustainable access to novel and existing antibiotics, there remain many challenges for both, low-and middle income countries and high income countries that can be efficiently addressed in a collaborative way.
- These include a diversification of manufacturing capacities, improving transparency and forecasting across distribution lines, establishing collaborative pooled procurement mechanisms and initiatives that could be developed among the United Nations, global procurers and other stakeholders to mitigate stockouts and shortages and introducing international platforms with access conditionalities and stewardship measures countries could subscribe to in order to access relevant antibiotics sustainably.
Selection of antibiotics
- Not only the quantity of antibiotic prescribed, but the selection of which antibiotic has a role to play in promoting drug resistance. Broad spectrum antibiotics target a larger range of bacteria and are more likely to select for resistance.
- Further research is needed to understand how to mitigate such knock-on effects. Innovative technical solutions are required to meet the need for new diagnostics — the longitude prize is one initiative rising to this challenge.
- Collaborative global efforts
- Although often viewed as a medical problem, antibiotic resistance is really one of managing a shared resource to maintain antibiotic effectiveness.
- Any conservation effort to protect this global resource would also necessarily need to be global.
- India — with its combination of large population, rising incomes that facilitate purchase of antibiotics, high burden of infectious diseases and easy over-the-counter access to antibiotics — is an important locus for the generation of resistance genes.
Global Efforts
Global Action Plan on Antimicrobial Resistance (GAP)
- Globally, countries committed to the framework set out in the Global Action Plan1 (GAP) 2015 on AMR during the 2015 World Health Assembly and committed to the development and implementation of multisectoral national action plans.
- It was subsequently endorsed by the Governing Bodies of the Food and Agriculture Organization of the United Nations (FAO) and the World Organisation for Animal Health (OIE).
- To ensure global progress, countries need to ensure costing and implementation of national action plans across sectors to ensure sustainable progress.
- Prior to the endorsement of the GAP in 2015, global efforts to contain AMR included the WHO global strategy for containment of Antimicrobial Resistance developed in 2001 which provides a framework of interventions to slow the emergence and reduce the spread of AMR.
World Antimicrobial Awareness Week (WAAW)
- World Antimicrobial Awareness Week reflect the broadened scope of WAAW to include all antimicrobials including antibiotics, antifungals, antiparasitics and antivirals.
- Held annually since 2015, WAAW is a global campaign that aims to raise awareness of antimicrobial resistance worldwide and encourage best practices among the general public, health workers and policy makers to slow the development and spread of drug-resistant infections.
|
Conclusion:
Although often viewed as a medical problem, antibiotic resistance is really one of managing a shared resource to maintain antibiotic effectiveness. Hence , addressing the challenge of excessive use while at the same time assuring sustainable supply of essential antibiotics is key to making health systems resilient to both COVID-19 and antimicrobial resistance